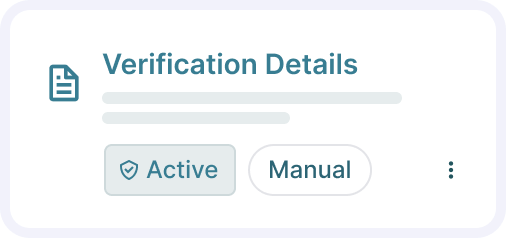
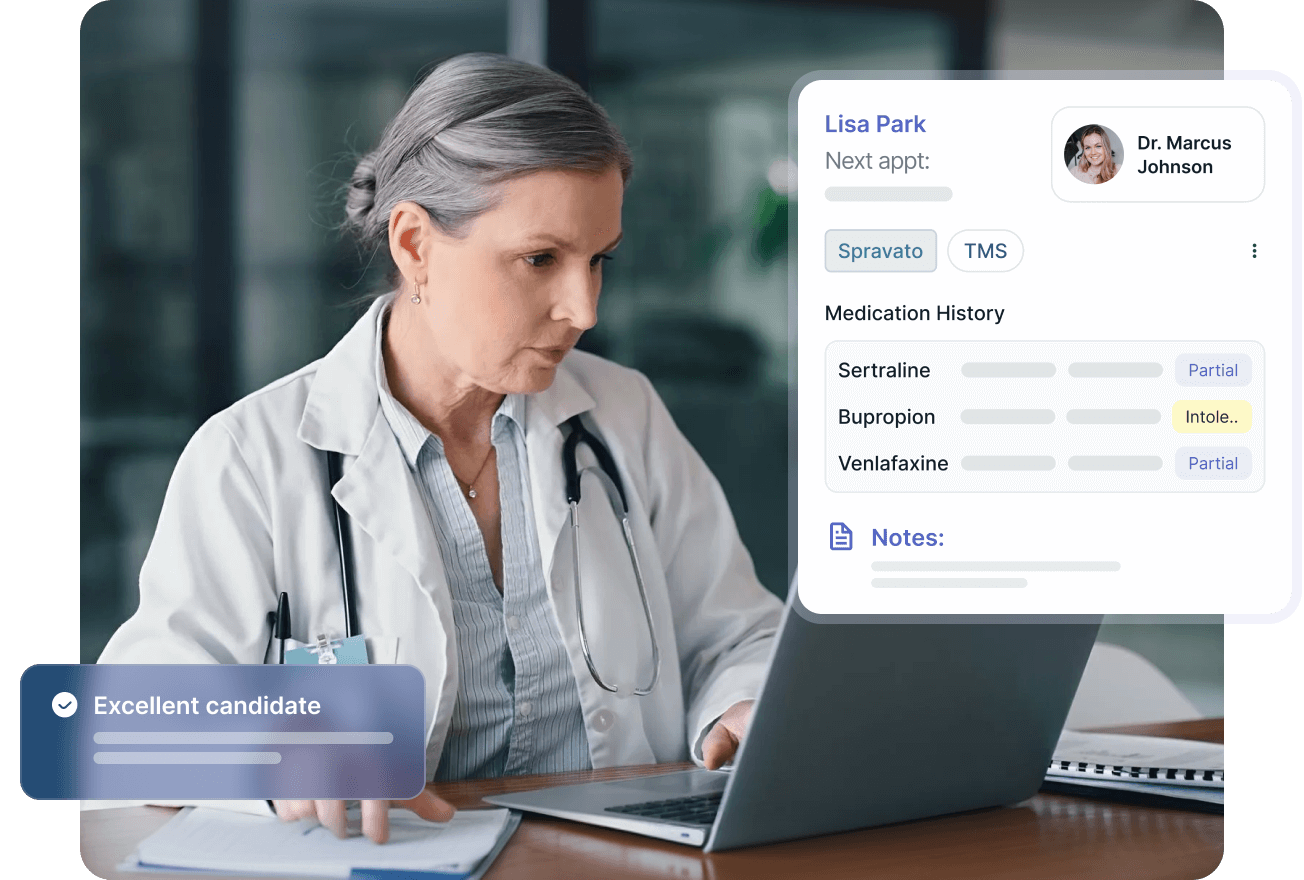
PRIOR AUTHORIZATION & BENEFIT VERIFICATION
Achieve 90%+ Prior Authorization Approval Rates
We handle prior authorization and benefit verification for behavioral health services including Spravato® and TMS with guaranteed 3-day submission and fast approvals, so your patients start treatment quickly.
.jpg)

Experts in navigating requirements for all major payers, including Medicare Advantage & Medicaid:



.png)

HOW IT WORKS
From Verification to Approval
Verify Coverage and Financial Responsibility
We confirm patient coverage upfront and include any relevant financial discounts and rebates in cost estimates to avoid surprises.
Build the Strongest Possible Case
We buy third-party data to enrich medical and medication history, then review clinical documentation to meet payer medical necessity criteria. If we identify denial risk, we provide feedback to course correct faster.
Submit and Fight for Approval
We submit requests within 3 days (most within 24 hours) and handle all payer communication. If denied, we fight and appeal endlessly, including conducting peer-to-peer reviews with payers.
Prior Authorizations Done Right
Proactive Approval Strategy

We buy third-party data to enrich medical and medication history before submission

We review clinical documentation and take action to strengthen cases before submission

We provide feedback if we identify denial risks so you can course correct faster
.png)
Guaranteed Fast Submission

We submit most prior authorizations within 24 hours, guaranteed within 3 days

We understand payer-specific criteria and denial triggers for Spravato® and TMS

We include relevant financial discounts and rebates in patient cost estimates upfront
Relentless Appeals Process

We fight and appeal every denial, including conducting peer-to-peer reviews with payors

We build strong clinical rationale to overturn denials and protect your revenue

We handle all payer communication so your staff can focus on patient care
.png)
FAQ
Your Questions, Answered with Clarity
How long does a prior authorization take?
01
Timing varies by payer, from days to weeks but our process minimizes delays by submitting them within 3 days.
What happens if a prior authorization is denied?
02
We start the appeals immediately, handling peer reviews and follow-up to overturn denials.
Do you handle benefit verification as well?
03
Yes, we verify benefits upfront to clarify coverage and patient costs.
Is this service included in your RCM platform?
04
Yes, prior authorization management is a core part of our Revenue Cycle Management solution.




.png)

