CREDENTIALING & CONCTRACTING
Get In-Network Faster with Better Rates
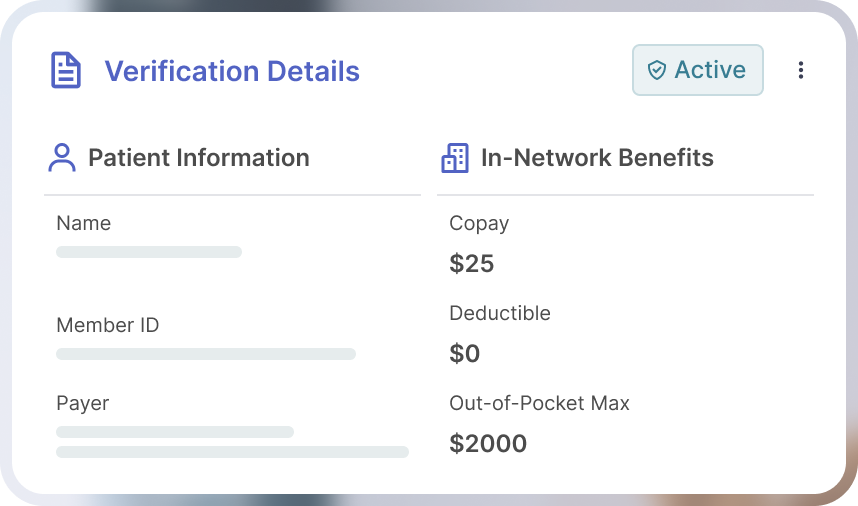
We manage credentialing and contracting for behavioral health clinics to get you in-network with major payers quickly and negotiate better reimbursement rates.
.jpg)
Get credentialed with major payers:



.png)

HOW IT WORKS
From Application to Contract
Build Your Payer Strategy
Our 100% US-based credentialing team analyzes your local market to identify which payers will drive the most revenue for your services and location.
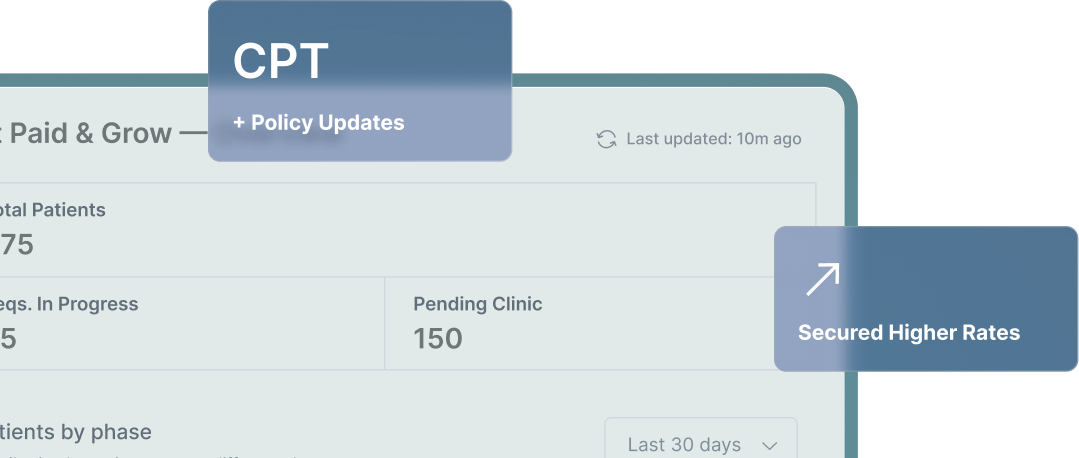
Complete Credentialing for All Clinicians
We submit applications with the right CPT codes to maximize Spravato® and TMS reimbursement, tracking every step to prevent delays.
Negotiate Contracts and Secure Better Rates
We leverage our network to negotiate favorable terms and enhanced rates, finding pathways in even when panels are closed.
Credentialing Built for
Interventional Psychiatry
.png)
Expert Credentialing Staff

100% US-based team with deep knowledge of interventional psychiatry billing

Direct communication with your clinicians throughout the credentialing process

Navigate complex payer requirements and documentation
Optimized for Spravato® & TMS

Ensure applications include the right CPT codes to maximize reimbursement for Spravato® and TMS

Understand payer-specific requirements for interventional treatments

Know how to get you in-network even when panels appear closed

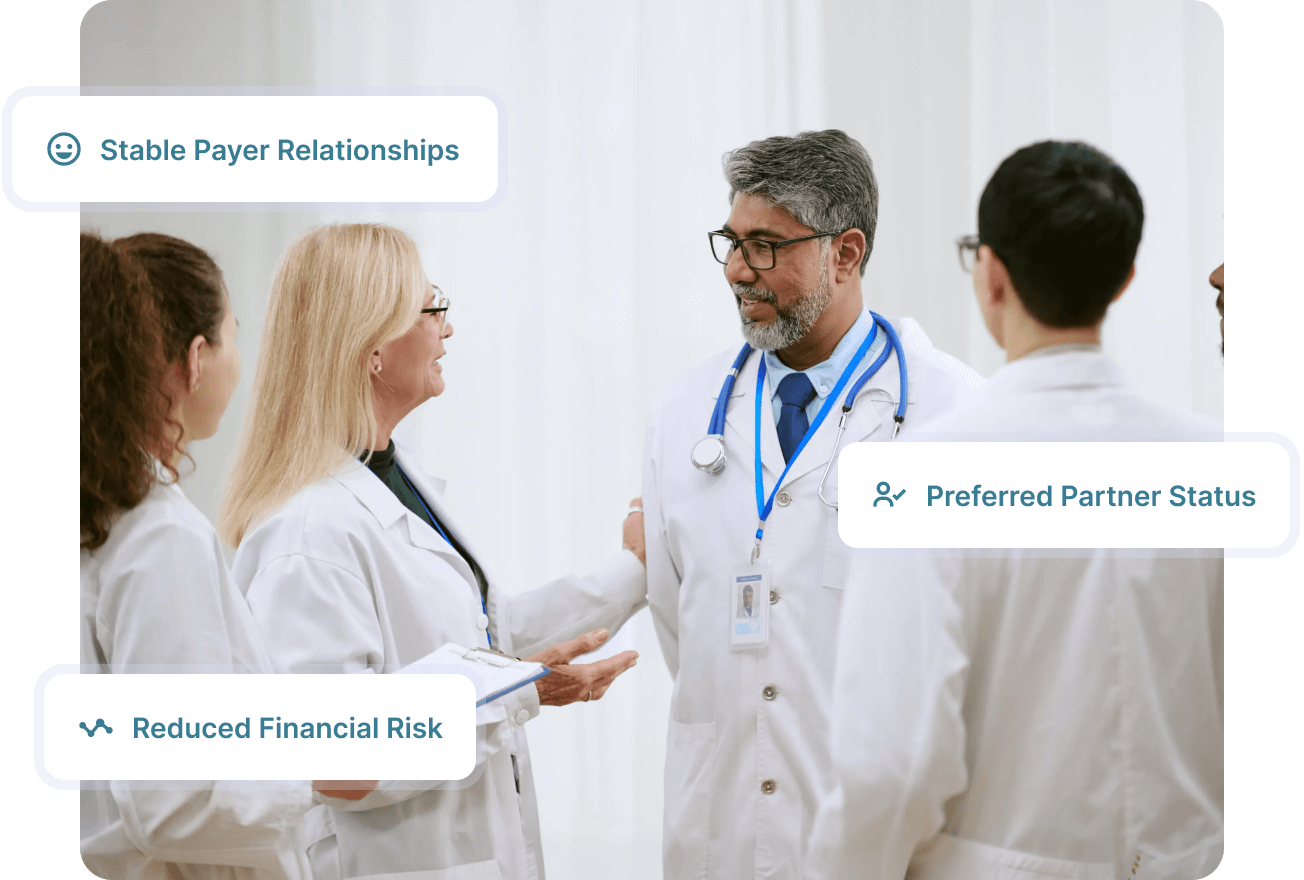
Network Leverage for Better Rates

Negotiate collectively to secure higher rates than individual practices can achieve

Use our payer relationships to find alternative pathways into closed panels

Secure contracts with favorable terms and enhanced reimbursement rates
Network Leverage for Better Rates
Big Leap Health negotiates as a network, securing higher rates than single practices can. This boosts your revenue while keeping your workflow simple.

.jpg)
FAQ
Your Questions, Answered with Clarity
What is the difference between credentialing and contracting?
01
Credentialing verifies clinician qualifications to join a payer network; contracting sets terms and reimbursement rates.
How long does credentialing take?
02
Typically 90-120 days; we help avoid delays that extend this timeline.
Can you help if I already started the process?
03
Yes, we take over stalled applications and manage them to completion.
What if a payer's panel is closed?
04
We explore exceptions and alternative pathways using our payer relationships.
Do you work with solo practitioners as well as group practices?
05
Yes, we support practices of all sizes, from solo to multi-site organizations.